Blog
Nov 14, 2025
How to Join the 3% of Agencies Winning the Home Health AI Revolution

Arvind Sarin
The Crisis Nobody Saw Coming
Right now, while you're reading this, a quiet revolution is transforming home healthcare. It's not happening in hospitals or tech companies. It's happening in agencies just like yours. Agencies that were drowning in referral chaos six months ago and are now capturing every opportunity. Agencies where nurses spent more time on documentation than patient care and now have hours back in their day. Agencies that couldn't hire fast enough to keep up with demand and have now increased capacity by 360% without adding a single full time employee.
The technology driving this transformation? Artificial intelligence.
But here's the uncomfortable truth. Only 3% of home healthcare agencies have successfully implemented AI solutions. The other 97%, perhaps including you, are watching from the sidelines, paralyzed by uncertainty, overwhelmed by options, or convinced that AI is either too expensive, too complicated, or too risky.
Meanwhile, the gap is widening every single day.
Your competitors are capturing the referrals you're missing. They're operating more efficiently with the same budget you have. They're attracting and retaining the clinical talent you desperately need. And they're doing it with AI systems that cost less than you're currently spending on pizza for staff appreciation events.
The question isn't whether AI will transform your agency. It's whether you'll lead the transformation or be forced to catch up after losing market share, revenue, and your best people to agencies that moved first.
This isn't about technology for technology's sake. This is about survival in a market where Medicare reimbursements aren't increasing, labor costs are climbing, and patient expectations are higher than ever. AI isn't the shiny new thing anymore. It's becoming table stakes.
The 3 Biggest Myths Killing Your AI Strategy
Before we talk about what's working, let's address the fears and misconceptions keeping 97% of agencies stuck.
Myth 1 "AI Will Replace My Nurses"
This is the most pervasive and damaging myth in healthcare AI. Let me be absolutely clear. AI doesn't replace clinicians. It amplifies them.
The data proves it. When agencies implement AI strategically, they don't see job losses. They see dramatic improvements in staff retention and satisfaction. One regional home health network we studied increased their operational capacity by 360% without hiring additional clinical staff. How? By eliminating the administrative cognitive load that causes burnout.
Think about what your nurses actually do in an 8 hour shift. If you're like most agencies, they spend 5+ hours on documentation, coordination, and administrative tasks for every 3 hours of actual patient care. That ratio is backwards, and everyone knows it. Your nurses didn't go to nursing school to wrestle with OASIS forms for 90 minutes per patient. They became nurses to care for people.
AI handles the repetitive, time consuming cognitive tasks that drain your clinical team. These tasks include reviewing charts, validating OASIS codes, scheduling coordination, documentation synthesis, and routine patient communication. This doesn't replace nurses. It returns them to nursing.
The agencies seeing 30% reductions in nurse turnover aren't replacing staff with AI. They're removing the friction that makes talented clinicians leave healthcare entirely.
Myth 2 "AI Costs $500,000 and Requires a Tech Team"
This myth persists because of enterprise software trauma. For decades, healthcare technology meant six figure implementations, 18 month timelines, and dedicated IT departments to keep systems running.
That world is gone.
Modern healthcare AI solutions run on subscription models ranging from $500 to $15,000 per month depending on your agency size. For a 100 patient agency, the true cost is typically $2 to $8 per patient per month. Let's put that in perspective. You're probably spending more on paper documentation supplies.
Even more remarkable. Many AI solutions can be configured and deployed in 30 minutes, not 18 months. No enterprise software installation. No dedicated servers. No IT department required. These are cloud based systems that integrate with your existing EMR through standard APIs that already exist in WellSky, KanTime, Alora, and every other major platform.
The agencies implementing AI successfully aren't hiring data scientists and building custom machine learning models. They're selecting proven solutions, connecting them to their existing systems, and seeing results within 30 to 60 days. The technical barrier that existed five years ago has collapsed.
Myth 3 "We Need to Wait Until AI Is More Proven"
This is the most expensive myth of all. The myth that waiting is safe.
Let's look at what "waiting" actually costs. Every month you delay, the following happens.
65% of your referrals leak because you can't respond fast enough to inquiries that come in after hours or when your intake coordinator is overwhelmed Your nurses spend 75% of their time on documentation instead of the patient care that improves outcomes and generates positive reviews Manual coding errors trigger claim denials that delay payment and risk compliance audits Chaotic scheduling wastes 2 to 3 hours daily per clinician in unnecessary drive time, contributing directly to the burnout that drives 25%+ annual turnover
These aren't future problems AI might solve someday. These are current costs AI is solving today at agencies that decided not to wait.
The "wait and see" strategy made sense in 2020 when healthcare AI was experimental. In 2025, it's organizational suicide. Early movers aren't taking risks. They're capturing advantages that compound monthly. The agency that implements an intake AI agent today doesn't just capture more referrals this month. They build a growth engine that widens the gap every single month while you "wait for more proof."
What's Actually Working Right Now. The Case Studies
Enough theory. Let's look at what's happening in real agencies with real results.
Case Study 1. Massachusetts General Brigham. Documentation Revolution
The Problem. Clinical staff spend more time on documentation than patient care, with nurses reporting documentation as their primary source of job dissatisfaction. The Solution. AI powered clinical documentation assistant that listens to patient interactions and generates structured clinical notes. The Results. 50% reduction in documentation time. Nurses who previously spent 45 minutes per patient on OASIS documentation now spend under 20 minutes. The time savings translated directly into capacity for additional patient visits without increasing staff. Perhaps more importantly, clinician satisfaction scores improved by 28 points in six months. The Key Insight. The AI doesn't replace the nurse's clinical judgment. It eliminates the mechanical transcription work that no one went to nursing school to do.
Case Study 2. Kaiser Permanente. Patient Access Transformation
The Problem. Average phone wait times of 18 minutes during peak hours, with 40% of callers abandoning before reaching a human. Staffing the phones 24/7 wasn't financially viable. The Solution. Conversational AI voice agents handling routine inquiries, appointment scheduling, and medication refill requests. The Results. Wait times dropped from 18 minutes to 30 seconds. Call abandonment fell to 8%. Patient satisfaction with phone interactions increased from 67% to 91%. The system handles 60% of all routine calls without human intervention, allowing staff to focus on complex cases requiring clinical judgment. The Key Insight. Patients don't care if they're talking to a human or an AI. They care about getting their problem solved quickly. For routine tasks, AI delivers a superior patient experience.
Case Study 3. iCare Home Health. 24/7 Referral Capture
The Problem. Missing 65% of referrals that came in outside business hours. By the time the intake coordinator followed up the next morning, potential patients had already been accepted by competitors. The Solution. An AI agent named "Nicole" handling after hours calls, conducting intake assessments, verifying eligibility, and routing urgent cases to on call staff. The Results. 60% of after hours calls are fully resolved without human intervention. Referral capture rate increased from 35% to 89%. The agency captured an additional $127,000 in revenue within 60 days. Referrals they would have lost entirely under the previous system. The Key Insight. You can't compete on business hours anymore. The agency that answers immediately, even at 2 AM, wins the patient.
Case Study 4. Cleveland Clinic. Predictive Readmissions
The Problem. Hospital readmission rates of 18% within 30 days of discharge, triggering Medicare penalties and harming patient outcomes. The Solution. Predictive AI analyzing patient data to identify high risk individuals before discharge, enabling targeted interventions. The Results. 30% reduction in preventable readmissions. The AI identified non obvious risk factors (medication adherence patterns, social determinants of health, subtle vital sign trends) that human clinicians missed. Each prevented readmission saved an average of $15,000 in direct costs. The Key Insight. AI doesn't replace clinical expertise. It sees patterns in data that humans physically cannot process.
Case Study 5. Regional Home Health Network. OASIS Liberation
The Problem. OASIS documentation consumes 90+ minutes per patient assessment, with error rates causing audit failures and claim denials. The Results. 75% time reduction, from 90 minutes to 25 minutes per assessment. Coding accuracy improved from 87% to 98%. Compliance audit performance improved from 82% to 96%. Nurses reported documentation as a minor stressor rather than their primary job frustration. The Key Insight. The blended workflow (AI handles the mechanical review and code suggestion, humans apply clinical judgment and oversight) outperforms either AI alone or humans alone.
The Common Thread
Notice what all these success stories share.
They focused on specific, measurable pain points (not vague "AI transformation") They kept humans in the decision making loop (AI augments, doesn't replace) They saw ROI within 60 to 90 days (not 18 month implementations) They started with one use case before expanding (pilot, prove, scale) They measured everything (hard metrics, not fluffy improvement claims)
This is the blueprint. This is what the 3% understand that the 97% don't.
The 3 Types of AI Every Agency Needs
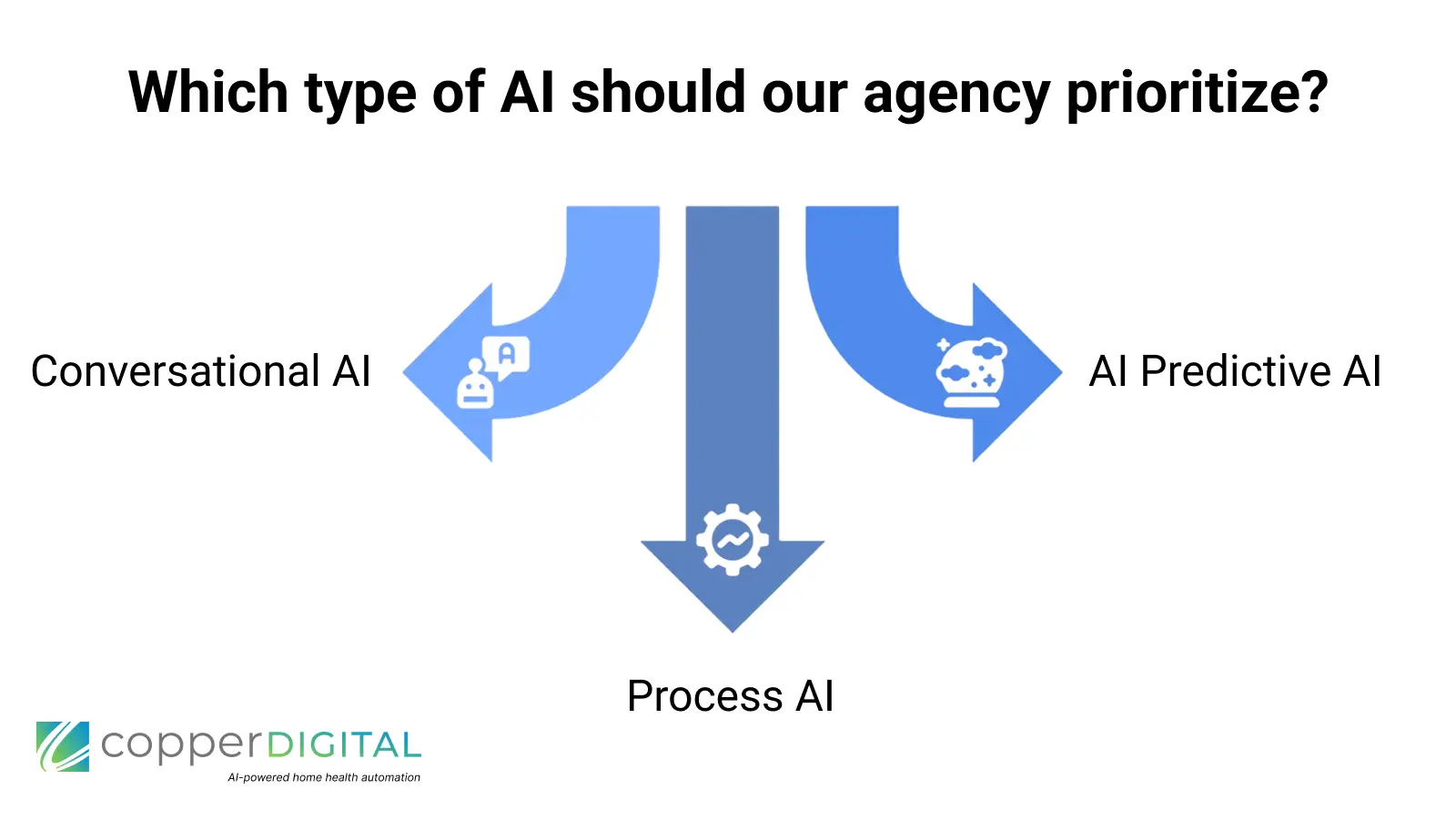
To understand how AI fits into your agency, you need to understand that "AI" isn't one thing. It's three distinct categories of technology solving three different classes of problems.
Type 1. Conversational AI (The Voice and Text Agents)
What It Does. Handles natural language conversations with patients, referral sources, and staff through voice calls, text messages, or chat interfaces. Real World Applications. After hours phone answering (60% resolution rate without human intervention) Referral intake and eligibility verification Appointment scheduling and reminders Routine patient check ins and symptom monitoring Provider relations and referral source communication Why It Matters. You physically cannot staff phones 24/7 with humans, but referrals don't stop coming at 5 PM. Conversational AI creates the always available, always responsive agency that patients and referral sources demand. Example. iCare's "Nicole" handles after hours calls with the same compassion and thoroughness as their best intake coordinator, capturing referrals that would otherwise go to competitors who happened to pick up the phone first.
Type 2. Predictive AI (The Crystal Ball)
What It Does. Analyze historical patterns in your data to forecast future outcomes and identify risks before they become problems. Real World Applications. Hospital readmission risk scoring Patient deterioration early warning systems Medicare denial prediction Staffing demand forecasting Revenue cycle optimization Why It Matters. Prevention is cheaper than reaction. Identifying a patient at high risk for readmission before discharge allows targeted interventions that cost hundreds instead of thousands. Predicting which claims will be denied before submission prevents the 45 day cash flow delay. Example. Cleveland Clinic's readmission prediction model catches patients who appear stable but have subtle risk factors (medication adherence history, living alone, pattern of vital signs) that human review misses. Each prevented readmission saves $15,000 in direct costs and preserves the patient relationship.
Type 3. Process AI (The Efficiency Engine)
What It Does. Automates repetitive cognitive tasks that follow consistent patterns. This is the work that humans can do but hate doing because it's mechanical and time consuming. Real World Applications. OASIS documentation review and code suggestion Chart review and medical record synthesis Prior authorization completion Billing and coding automation Schedule optimization and route planning Why It Matters. Your most expensive resource is skilled clinical time. Every hour a nurse spends on mechanical documentation is an hour not spent on patient care. Process AI returns clinicians to clinical work. Example. The regional network's OASIS AI doesn't make clinical judgments. It reviews the clinician's notes, suggests appropriate codes based on documented findings, and flags inconsistencies for human review. The nurse maintains full oversight but reclaims 60+ minutes per patient.
Your First Action Step. The 10 AI Opportunities Exercise
Here's something practical you can do right now, before you invest a dollar in AI technology. Identify your 10 highest value AI opportunities.
Grab a notepad and walk through your agency's operations with four questions.
Question 1.
What Tasks Are Repetitive? List every task your team does multiple times per day that follows a consistent pattern. Examples. answering the same questions about your services, verifying insurance eligibility, scheduling appointments, reviewing charts for OASIS compliance.
Question 2.
What Tasks Are Time Consuming? Identify the activities that consume disproportionate time relative to their value. Examples. OASIS documentation taking 90 minutes, phone tag with referral sources, manually optimizing daily schedules.
Question 3.
What Tasks Are Error Prone? Find the places where human variability causes problems. Examples. coding inconsistencies triggering denials, missed patient follow ups, documentation gaps causing audit failures.
Question 4.
What Needs to Happen 24/7? Identify the requirements that don't respect business hours. Examples. after hours referral inquiries, patient emergencies, urgent scheduling changes, weekend coordination.
Once you've brainstormed answers to all four questions, you'll likely have 20-30 items on your list. Now prioritize them using this simple framework.
High Value = (Frequency × Time Cost × Error Rate) + Strategic Importance
Your top 10 opportunities are likely After hours call handling OASIS documentation review Referral intake and eligibility verification Schedule optimization Prior authorization completion Patient appointment reminders Provider communication and updates Chart review for billing Quality measure tracking Staff coordination and communication
Notice something? Every single one of these has proven AI solutions available today, with documented ROI in real agencies.
The Window Is Closing (But It's Not Closed Yet)
Let's talk about competitive dynamics.
In 2020, AI in home healthcare was experimental. Early adopters were taking genuine risks. In 2022, AI was promising but unproven at scale. In 2023, the evidence started becoming undeniable. In 2024, the case studies multiplied.
We're now in 2025, and we've crossed the threshold. AI in home healthcare is no longer experimental. It's proven, it's accessible, and it's becoming expected.
Here's what this means for you.
The early mover advantage window is still open, but it's closing fast. Agencies implementing AI today are building advantages that compound monthly.
The referral advantage. Every month with 24/7 intake AI, you capture patients your competitors miss The efficiency advantage. Every month with documentation AI, your nurses have capacity for more visits. The talent advantage. Every month with scheduling AI, your staff retention improves while competitors' deteriorates. Every month of AI captured data gives you better insights and better predictions
These advantages don't just add. They multiply. The agency that captures more referrals generates more revenue to invest in better AI tools. Better tools attract better talent. Better talent delivers better outcomes. Better outcomes generate more referrals.
Meanwhile, agencies still "waiting and seeing" fall further behind every month. The gap isn't linear. It's exponential.
But here's the good news. You're not too late. 97% haven't moved yet. Your local competitors probably haven't implemented AI successfully. You can still be the first in your market to offer 24/7 intake, sub 5 minute OASIS review, or predictive scheduling.
The window is closing, but you're reading this right now, which means you're still in the game.
Your Next Step. Join the 3%
Everything you've read in this article, the case studies, the cost realities, the specific AI applications, the opportunity identification framework, is just the beginning.
The 3% of agencies successfully implementing AI have something the other 97% don't. A complete roadmap from understanding to implementation.
They know Which AI technology to implement first (based on their specific pain points, not generic advice) How to evaluate vendors without getting lost in marketing hype What questions to ask during demos to separate real capabilities from vaporware How to get staff buy in instead of resistance How to integrate AI with their existing EMR without IT drama How to measure ROI accurately How to pilot safely before scaling broadly How to navigate HIPAA, FDA, and compliance requirements How to build the business case that gets board approval
Over the past three years, we've helped more than 500 home healthcare leaders navigate this exact transformation, from AI curious to AI powered. We've documented what works, what fails, and why. We've built the frameworks, the checklists, the vendor comparison tools, and the implementation playbooks.
Now we've compiled everything into a comprehensive training program. The AI Home Healthcare Mastermind.
What You'll Get.
15 Comprehensive Modules covering Foundation Phase (Modules 1 to 4). Demystifying AI, understanding the current landscape, hands on tool exploration, strategic thinking frameworks Implementation Phase (Modules 5 to 10). Addressing staff fears, reclaiming time with documentation AI, building ROI cases, mastering voice AI, solving staffing challenges, preventing denials Specialization Phase (Module 11). Role specific tracks for administrators, clinicians, and operations leaders Scale Phase (Modules 12 to 15). Pilot program design, change management mastery, compliance and ethics, 3 year transformation roadmap
Real Implementation Tools. Vendor evaluation frameworks (stop wasting time with the wrong solutions) 90 day implementation roadmap (know exactly what to do, when) ROI calculator customized for home healthcare (prove the value to your board) Staff communication templates (turn skeptics into champions) Compliance checklists (stay on the right side of HIPAA and FDA)
Live Expert Access. Monthly Q&A sessions with AI healthcare experts Private community of peer agencies implementing AI Direct support during your implementation
Lifetime Access. All future updates as AI capabilities evolve New modules added at no additional cost Permanent access to community and resources
This isn't theoretical education from academics who've never run a home health agency. This is the practical, battle tested playbook from frontline implementation with real agencies seeing real results.
The Investment.
Most healthcare organizations spend $50,000 to $500,000 on AI consultants who deliver theoretical frameworks without practical implementation. Then they waste another 12 to 18 months trying to figure out what actually works.
The AI Home Healthcare Mastermind is $997 one time payment (or 3 payments of $347).
One enrollment covers unlimited team members at your organization. Bring your leadership team, clinical managers, and operations directors. Shared understanding accelerates implementation.
The Guarantee.
Your success is completely guaranteed. Enroll in the course. Go through the training. Implement the frameworks. If you don't see a clear path to transforming your operations with AI within 60 days, we'll refund every penny. No questions asked.
You're not risking anything. The only risk is staying where you are while competitors gain ground with AI that works.
Ready to Join the 3%?
The AI revolution in home healthcare is happening with or without you. Your competitors are deploying AI agents that automate intake, optimize scheduling, and accelerate documentation.
They're capturing referrals you're missing. They're operating more efficiently with the same budget. They're attracting and retaining the clinical talent you need.
The gap is widening every single day.
You have two choices.
Wait and hope that AI will somehow not impact your organization, your market share, or your operational viability. (Spoiler. It already is.) Take action now with proven strategies, implementation blueprints, and expert guidance that transforms AI from scary buzzword into competitive advantage.
The window for early mover advantage is closing. But it's not closed yet.
Your organization's future depends on the decision you make in the next 10 minutes.
Enroll in The AI Home Healthcare Mastermind Now →


