Blog
Jan 2, 2026
How AI Agents and Predictive Analytics Are Rewriting the Rules of Home Health

Arvind Sarin
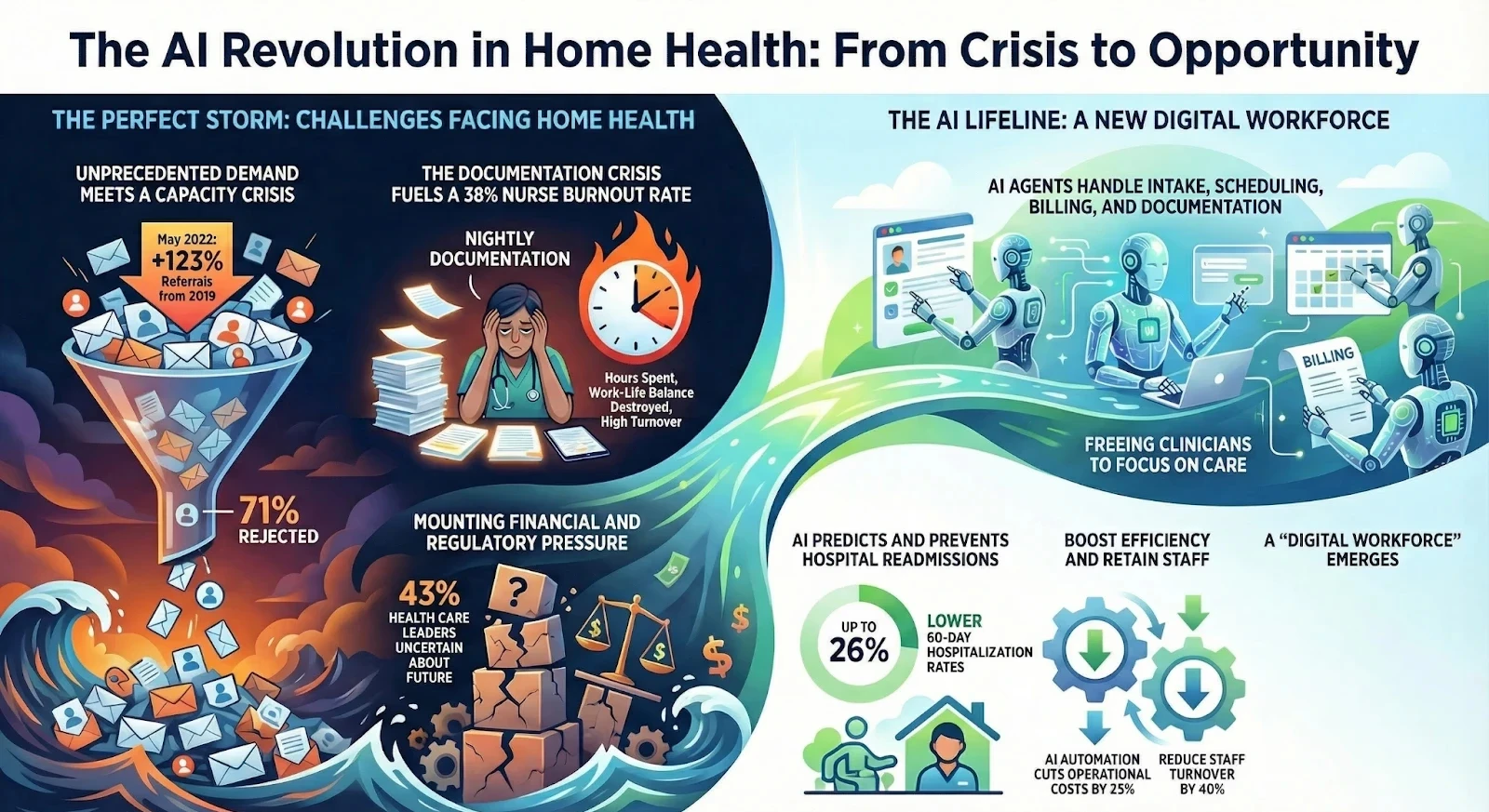
The home health industry is currently navigating its most difficult era in decades. We are facing a convergence of challenges that some call the perfect storm. The Silver Tsunami of aging patients is driving demand to record highs while the clinical workforce is shrinking.
The 2026 Healthcare Industry Outlook confirms this reality as executives explicitly state that customers do not have enough people capacity to meet demand. We can no longer solve these problems simply by hiring more people because there are no people to hire.
The solution lies in a fundamental shift in how we operate. We are moving away from static software tools and entering the era of the Digital Workforce.
From Passive Software to Active AgentS
For the last twenty years, technology in home health meant Electronic Medical Records. These systems are passive databases. They wait for a human to input data, click buttons, and run reports.
The new transformation is the rise of AI Agents. According to new data, 78% of healthcare executives now believe that future competitiveness hinges entirely on leveraging AI to reimagine operations. However, only 22% of organizations have figured out how to use it effectively. This gap represents a massive opportunity for agencies willing to move first.
Consider the role of intake. In the traditional model, a human coordinator must answer the phone, write down details, and manually enter them into the EMR. If the phone rings while they are on another line, the referral is lost.
In the AI model, an agent like Nicole functions as an infinite intake department. She answers the phone instantly and validates insurance in real time. This is not just automation. It is the deployment of a digital employee who never sleeps.

Predictive Analytics as the New Clinical Director
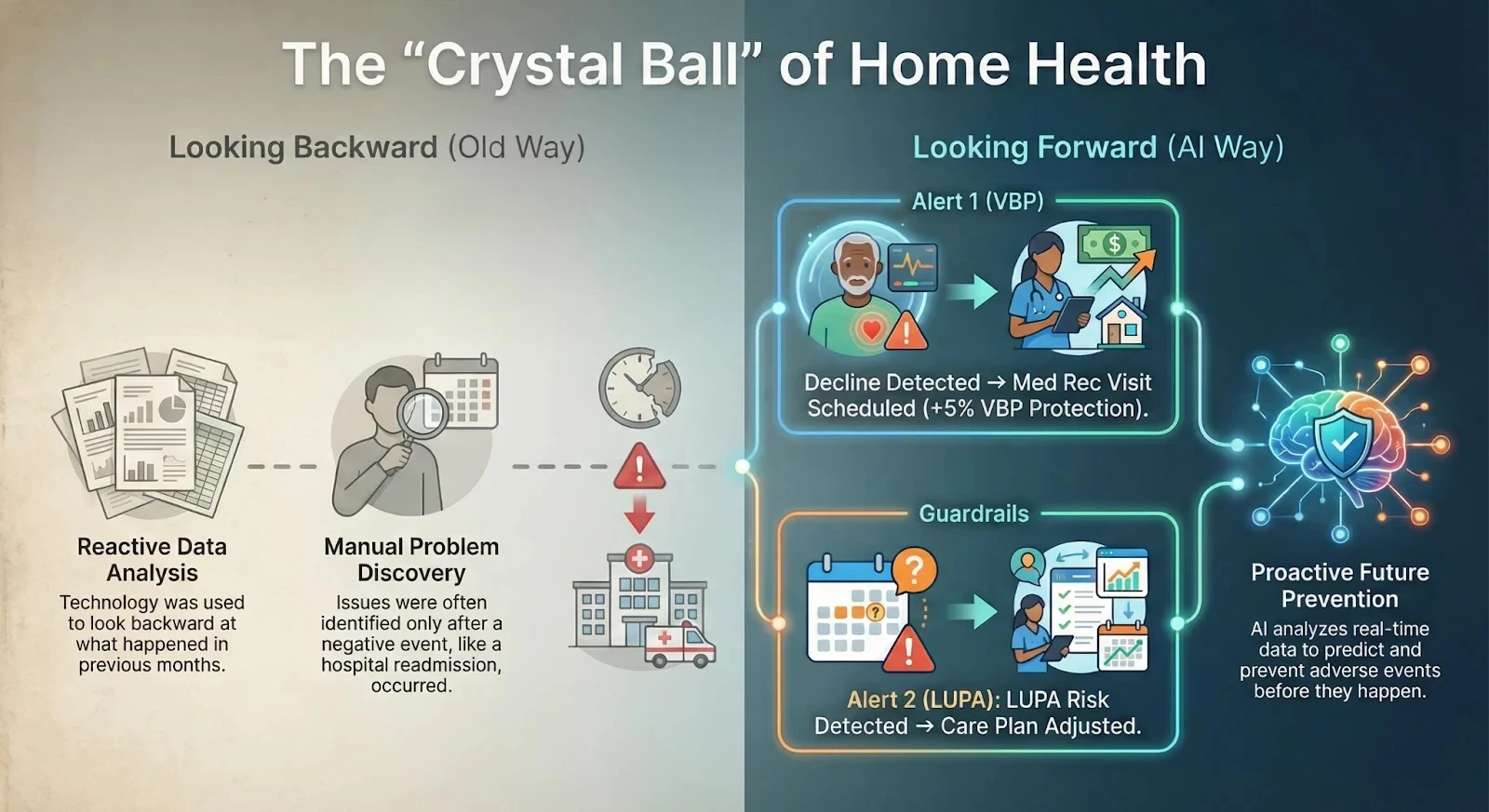
Data has always existed in home health, but it has largely been used to look backward at what happened last month. The revolution today is using that data to look forward.
This shift is accelerating rapidly, with a reported 33% increase in the industry's focus on connected care models for 2026. By analyzing thousands of data points from patient history and real-time visit notes, AI can now predict adverse events before they happen.
Preventing Readmissions
AI models can scan clinical notes for subtle keywords that indicate a decline in patient condition, which a human reviewer might miss. The system can flag a high-risk patient and suggest a medication reconciliation visit. This directly impacts your VBP scores, which now determine up to a 5% positive or negative adjustment on your Medicare payments starting in 2025.
Eliminating LUPA
Low Utilization Payment Adjustments are silent revenue killers. Predictive models track the visit utilization against the episode timing. The AI acts as a guardrail that alerts the scheduler when a patient is at risk of falling into a LUPA bracket so the agency can adjust the care plan immediately.
Solving the Documentation Crisis
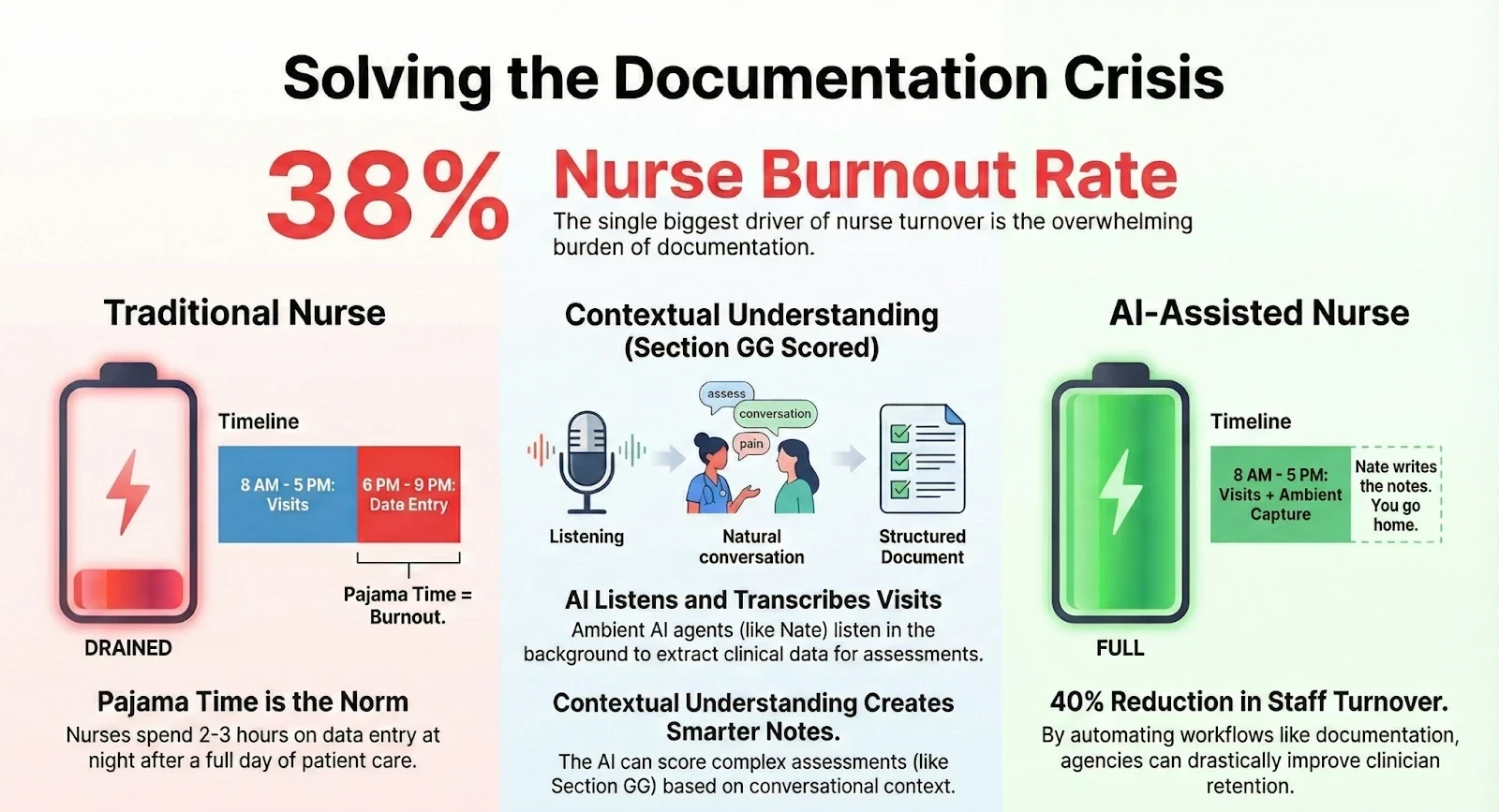
The single biggest driver of nurse turnover is documentation. We ask clinicians to work a full day seeing patients and then spend two to three hours at night acting as data entry clerks.
This leads to a staggering 38% burnout rate among nurses. This pajama time destroys work-life balance and forces talented clinicians out of the industry.
This is where ambient AI technology is changing the game. Agents like Nate utilize large language models to listen to the patient visit in the background. They filter out the casual conversation and extract the hard clinical data needed for the OASIS assessment.
The impact here is profound. The AI understands the context of the conversation. It can score functional impairments for Section GG based on what it heard rather than relying on default templates. This returns the nurse to the bedside and turns documentation into a review process rather than a creation process.
The Financial Firewall
The revenue cycle is the heartbeat of any agency. The traditional approach is reactive, where billing teams chase down denials after the claim has been rejected. The modern AI approach is proactive.
AI Agents like Maria serve as a financial firewall at the front door. By analyzing referral documents and running them against payor rules instantly, these agents identify missing authorizations and coding errors before the patient is even scheduled.
This moves the revenue cycle from a chase and collect model to a clean claim model. With margins under pressure from rising labor costs, automating this front-end work is essential for survival.
The Agency of the Future
The future of home health is not about replacing humans. It is about elevating them. When we let AI Agents handle the repetitive tasks of scheduling, intake coding, and data entry, we free our human staff to do what only humans can do.
We free our nurses to heal. We free our therapists to rehabilitate. We free our owners to grow.
The technology is no longer theoretical. It is here today, and it is working. The agencies that adopt this digital workforce will be the ones that survive the staffing crisis and thrive in the years to come.


