Blog
Dec 1, 2025
Why Your Referral Management Process Costs You Admissions

Arvind Sarin

If you placed a stopwatch on your intake desk right now, how long would it take to process a single referral?
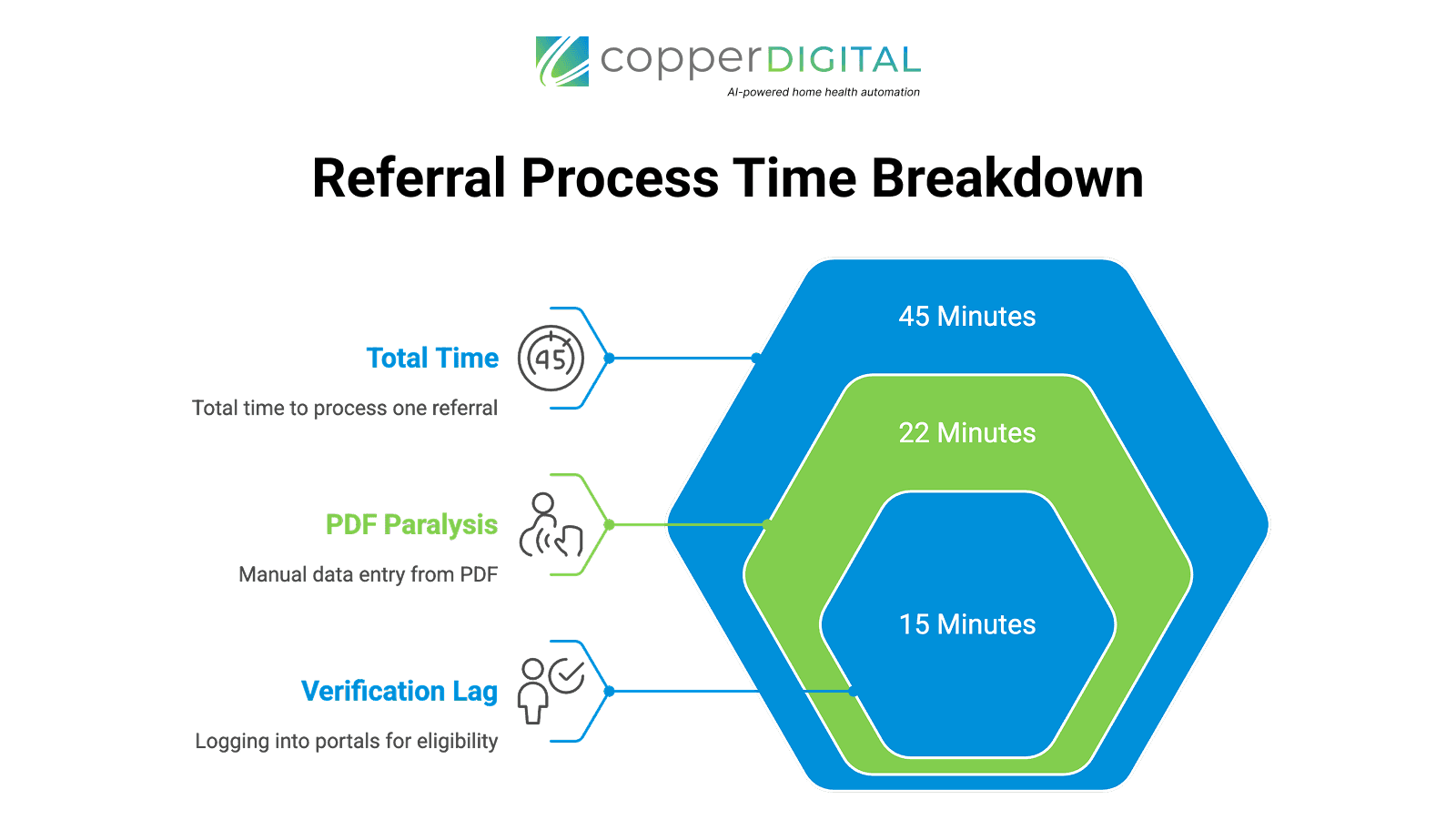
We measured this across 50+ mid-sized home health agencies. The average is 45 minutes from the moment the fax hits the inbox to the moment the patient is marked as "Ready to Schedule" in Homecare Homebase or WellSky.
In that 45-minute window, three things happen:
You are manually re-typing data.
You are sitting on hold with a payer.
Your competitor has already called the patient.
Referral sources, such as hospitals, SNFs, and discharge planners, do not choose agencies based on clinical outcomes. They choose the agency that says "Yes" the fastest. If your referral management process is stuck in the 45-minute slow lane, you aren't losing to "better" agencies. You are losing to faster ones.
Here is where the time (and revenue) is actually leaking, and how to fix it.
Bottleneck 1: The PDF Paralysis
The vast majority of home health referrals still arrive via fax or e-fax. This creates a data trap.
Your intake coordinator receives a 20-page PDF from the hospital. To get that patient into your EMR, they have to open the PDF on one screen and your EMR on the other, then manually type:
Patient Demographics
Insurance IDs
Diagnosis Codes (ICD-10)
Medication Lists
Referral Source Details
The Cost This manual data entry takes an average of 22 minutes per referral.
The Risk A single typo in the Member ID or Date of Birth triggers a claim denial 30 days later. According to healthcare denial statistics, inaccurate patient data is a leading cause of revenue loss
Many agencies try to solve this with basic "screen scraping" bots, but as we discussed in Why RPA Fails in Home Health, these brittle bots crash the moment your EMR pushes a UI update. You don't need a bot that blindly clicks buttons. You need a system that reads the document.
The Fix Intelligent Document Processing (IDP). Modern intake software doesn't just "scrape" the screen. It extracts the data from the unstructured PDF and pushes it directly into the EMR fields in seconds, not minutes.
Bottleneck 2: The Verification Lag
Once the data is typed in, the real delay begins with Eligibility Verification.
In the traditional workflow, your intake staff has to log into a payer portal (e.g., Availity, Optum) or, worse, pick up the phone and call the insurance company. They sit on hold to answer three questions:
Is the coverage active?
Is home health a covered benefit?
Is authorization required?
The Cost: This process eats up 15–20 minutes per patient.
The Reality: While your staff is on hold with Blue Cross, the discharge planner at the hospital is calling the next agency on their list because you haven't confirmed acceptance yet.
The Fix Automated Eligibility Checks. Your referral management system should run an instant "ping" to the clearinghouse the second the patient data is extracted. You should know if the patient is eligible before a human even reviews the file. This aligns with CMS guidelines for timely initiation of care.
Bottleneck 3: The After-Hours Black Hole
This is the silent killer of agency growth.
Data shows that roughly 40% of referrals and inquiries occur after 5:00 PM or on weekends.
Scenario A: You pay an answering service to take a message. The message sits in an inbox until 8:30 AM Monday.
Scenario B: You pay an on-call nurse overtime to answer the phone, burning them out with administrative tasks.
By the time Monday morning rolls around, that Friday night referral has often been picked up by a competitor who had 24/7 intake coverage.
As detailed in our breakdown of AI Voice Agents in Home Health, the solution isn't hiring a night shift. It's using Voice AI that can actually process the referral-taking the details, checking the calendar, and queuing the admission-without waking up your clinical director.
The Math: What is 42 Minutes Worth?
We have helped agencies reduce their intake cycle from 45 minutes to 3 minutes.
This isn't just about saving administrative time (though that is nice). It is about Capacity to Grow.
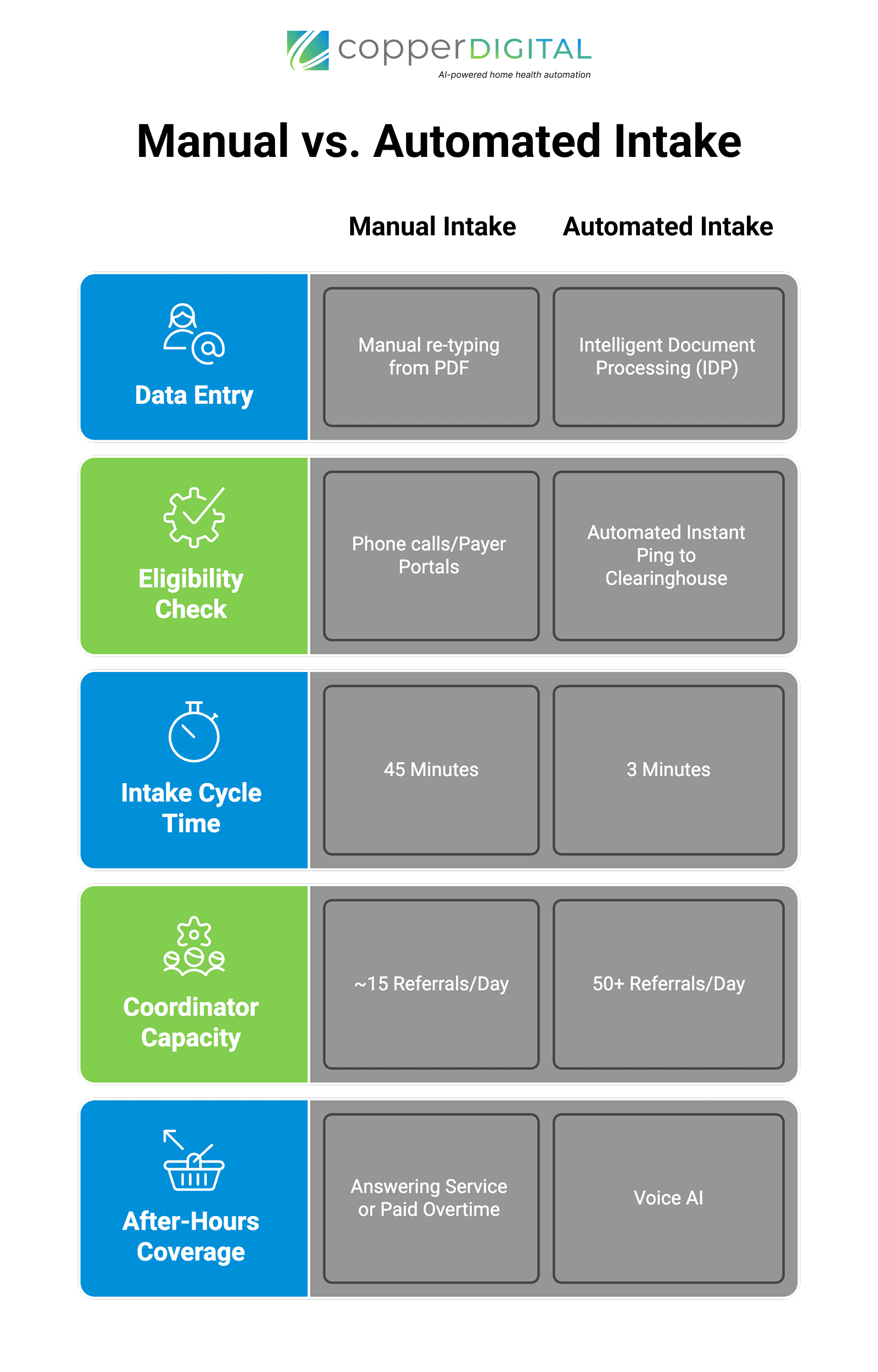
Manual Intake: One coordinator caps out at ~15 referrals a day. If you want to grow, you have to hire more admin staff, eating into your margins.
Automated Intake: That same coordinator can handle 50+ referrals a day because they are only managing exceptions, not doing data entry.
When you remove the friction, you remove the invisible ceiling on your revenue.
Stop Losing Referrals to Data Entry
Your clinical care is excellent. Don't let a slow back office prevent patients from experiencing it.
CopperOne automates the entire referral management chain-extraction, verification, and EMR entry-so you can say "Yes" while your competitors are still typing.
Book a Demo: See Your Intake Reduced to 3 Minutes

